Health experts are calling for Female Genital Schistosomiasis (FGS) services to be fully integrated into sexual and reproductive health and rights (SRHR) programs, warning that the neglected disease continues to harm women and girls in high-prevalence regions.
What is FGS?
According to the World Health Organization (WHO), FGS occurs when parasites released by freshwater snails penetrate the skin during contact with infested water. Once in the body, the parasites develop into worms that lodge in blood vessels. Their eggs can become trapped in the female reproductive tract, causing scarring, ulcers, pain, and bleeding.
If untreated, FGS can lead to infertility and increases the risk of HIV, Human Papilloma Virus (HPV), and cervical cancer.
Why Integration Matters
FGS is often misdiagnosed as a sexually transmitted infection (STI) due to overlapping symptoms. This misdiagnosis leads to incorrect treatment, stigma, discrimination, and gender-based violence (GBV).
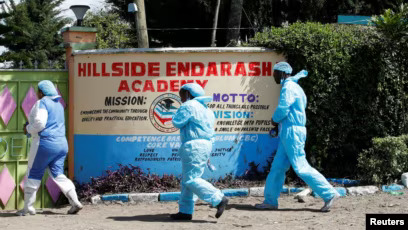
A new study conducted in Homa Bay, Kwale, and Kilifi counties by LVCT Health, in partnership with Frontline Aids, Bridges to Development, and funded by the Children’s Investment Fund Foundation (CIFF), found that integrating FGS into SRHR services is the most effective way to control and prevent the disease.
“In the process of screening for cancer, you are also screening for FGS. It does not add workload, since both reports can be written together,” said a healthcare worker in Homa Bay, noting that integration was both feasible and practical.
Key Findings from the FGS Integration Report
- FGS remains relatively unknown and misunderstood, even in high-risk areas.
- Awareness campaigns are critical to help both communities and healthcare workers identify and manage the disease.
- Healthcare workers can play a crucial role in diagnosing, treating, and offering psychosocial support to women facing stigma.
- Integration aligns with global health funding priorities, which are moving away from siloed disease interventions toward holistic care.
What Needs to Be Done
Experts warn that integration will only succeed if:
Experts warn that integration will only succeed if:
- Clinical staff receive specialized training and supportive supervision.
- Health facilities are supplied with diagnostic tools.
- Praziquantel, the primary drug for treating FGS, is readily available in all affected counties.
By embedding FGS services into SRHR programs, Kenya can not only improve early detection and treatment, but also protect women and girls from the long-term health, social, and economic consequences of this neglected disease.
“Integrating FGS into SRHR is not optional, it’s essential if we are to protect women’s health and rights,” the report concludes.